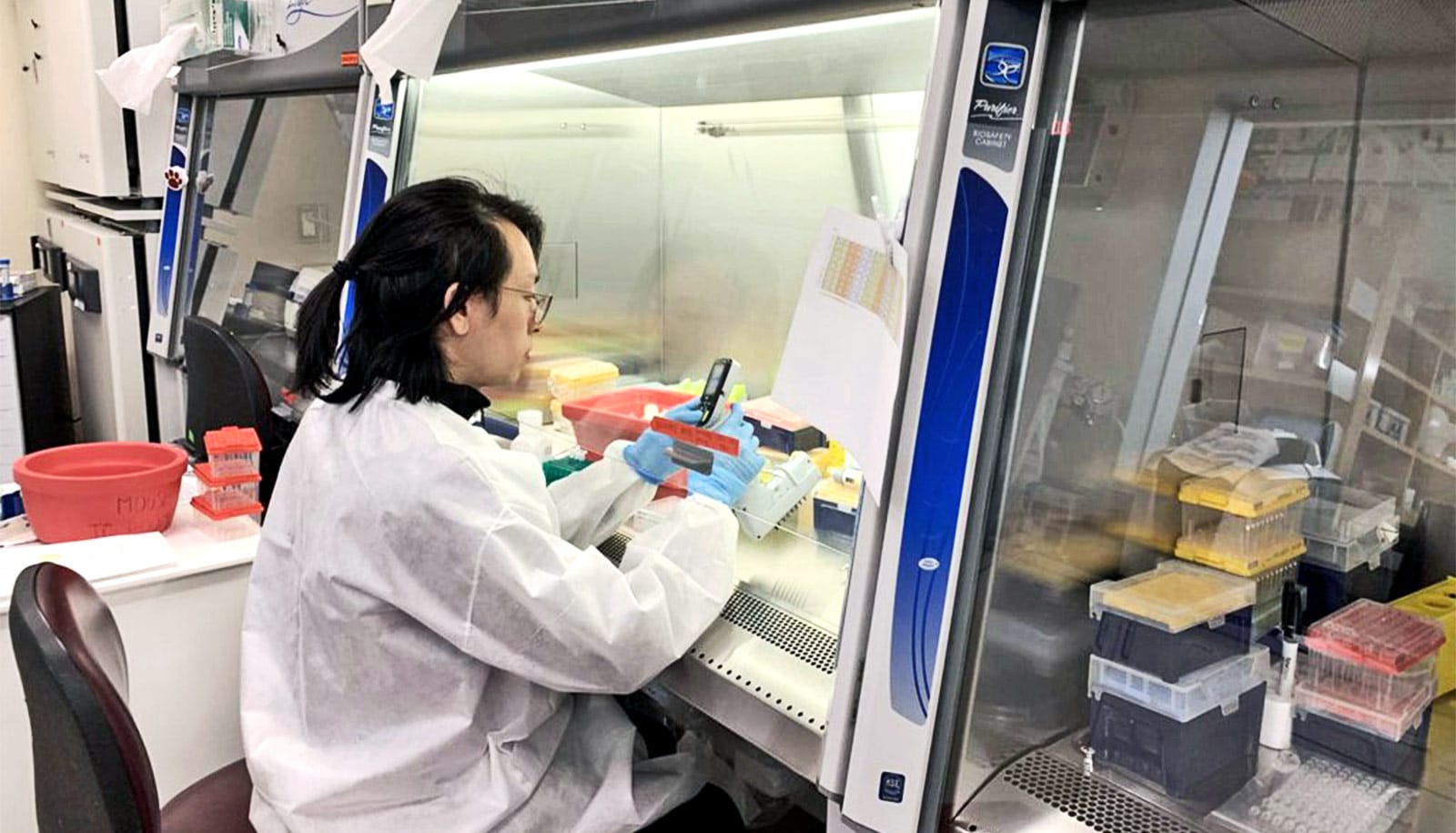
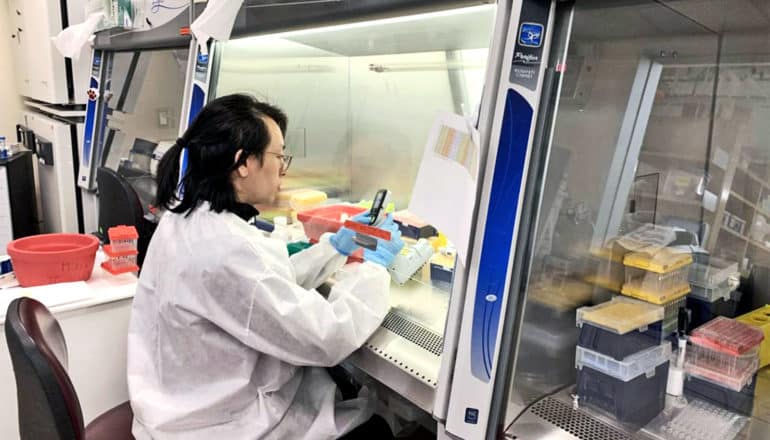
Working with a patient sample, CReM researcher Anthony Yeung performs PCR to search for SARS-CoV-2 RNA, genetic material unique to the novel coronavirus that would indicate a positive result for COVID-19 infection. (Credit: Boston U.)
Team creates their own coronavirus test to fill gaps
"If we can [get a] result faster, that also protects our friends and loved ones... who are going into the clinic. My best friends are going to war."
A team has created their own coronavirus test to address shortages in testing capacity.
Scrolling Twitter late at night on March 12, Boston University’s George Murphy noticed a desperate tweet coming from the feed of his friend and fellow researcher, Lea Starita of the University of Washington. She was asking for lab-savvy volunteers to help process coronavirus tests that had been jury-rigged by the Seattle Flu Study.
“If you’re coming up with a test result that will lead to clinical decisions, it has to be right…”
As the two scientists began exchanging direct messages about what was happening in Seattle—the first US epicenter to emerge in the spread of the SARS-Cov-2 virus responsible for COVID-19 infections—Murphy, codirector of the Center for Regenerative Medicine (CReM) on Boston University’s Medical Campus, felt a dawning realization that the same fate would soon be upon the Greater Boston area and the university’s own teaching hospital, Boston Medical Center (BMC).
Across the nation, and the city of Boston, there would not be enough coronavirus tests from the Centers for Disease Control and Prevention (CDC) to go around. Researchers and clinicians would need to develop their own clinically validated tests to have a fighting chance.
“She was telling me her war story of having to do inhouse testing, navigating governmental restrictions,” Murphy says. “It got me thinking, maybe we should be thinking about trying to do something here.”

‘Standing up’ a new coronavirus test
The next day, March 13, Murphy met with Chris Andry, chair of pathology at the School of Medicine and BMC.
“We hatched a plan to try and ‘stand up’ our own [coronavirus test],” Murphy says. Stand up, in the clinical world, describes the complex process to get a new diagnostic test validated and approved according to the stringent regulations of the US Food and Drug Administration. “If you’re coming up with a test result that will lead to clinical decisions, it has to be right,” he says.
Murphy and Andry’s meeting kicked off a week-plus-long flurry of around-the-clock activity, as CReM researchers—most of their own experiments already shuttered by social distancing efforts—volunteered in droves to design an inhouse COVID-19 test from scratch. They joined forces with a team of clinical lab technicians led by Nancy Miller, chief and vice chair of BMC laboratory medicine. They also leaned on the expert advice of fellow scientists at Massachusetts General Hospital, the Broad Institute of MIT and Harvard, and the University of Washington.
“My best friends are going to war.”
All told, more than 50 volunteers swarmed to the CReM from across the BU Medical Campus, working in shifts to ensure proper social distancing. By the week’s end, their teamwork culminated in a one-of-a-kind coronavirus test that can spit back a positive or negative result in less than 24 hours. The crew of collaborators is now processing many dozens of such tests each day—performing all of BMC’s COVID-19 testing—and making plans to even further ramp up capacity.
“We repurposed the whole CReM,” Murphy says of the state-of-the-art stem cell lab. Overnight, its researchers converted the facility into a makeshift command center and prototyping assembly line for coronavirus testing. Meanwhile, at BMC, patients began surging into the hospital with symptoms fitting the profile for the novel coronavirus. Clinicians faced agonizingly long delays waiting for patients’ COVID-19 test results, relying on state and commercial labs to validate swabs within five to seven days.
“It’s dangerous for healthcare workers if they are unaware someone they are treating has the coronavirus,” Murphy says. “That’s data that clinicians need to make decisions, to either quarantine patients or whether to use precious, dwindling supplies of [personal protective equipment] when they don’t need to. If we can [get a] result faster, that also protects our friends and loved ones from the CReM and around campus who are going into the clinic. My best friends are going to war.”
‘Heroic effort’
One of those friends includes the CReM’s director, Darrell Kotton, a stem cell biologist, Boston University School of Medicine professor of medicine, and a pulmonary/critical care physician at BMC. He reported into BMC’s intensive care unit on Wednesday, March 25, to serve as an attending physician alongside other doctors and physician-scientists from the BU Medical Campus community. There, he is doing everything he can to keep patients alive who have gone into respiratory failure from COVID-19 infection.
“…it’s been an exceptional and heroic effort—it’s made a big difference for the hospital, clearing a key early hurdle that faced us…”
“When the first patients were being admitted to BMC with COVID-19, we had a system meltdown in testing bandwidth,” Kotton says. “Tests being sent out that weren’t being turned around [quickly]. The hospital was getting bogged down. So I was thrilled when George’s team stepped in.”
He knew that since CReM researchers work with molecular reactions every day, Murphy’s team could help. “[Seeing them team up] with Chris, it’s been an exceptional and heroic effort—it’s made a big difference for the hospital, clearing a key early hurdle that faced us,” Kotton says.
To start, the collaborators filed what’s called an Emergency Use Authorization (EUA), an application released by the FDA that allows for research medical centers and commercial companies to develop their own inhouse COVID-19 tests and protocols for emergency FDA approval. Across the country, “everybody is trying to do it,” Murphy says. The idea is that you develop and “vet the diagnostic [test] in a research setting, and then move it up to clinical standards.”
Challenges and pitfalls
From the get-go, the team faced several choke points that threatened its ability to get an inhouse test off the ground. One of the first steps in testing for coronavirus is to use a reagent, called a viral RNA extraction kit, to break free the unique and identifying genetic strands of the SARS-Cov-2 virus from cells swabbed out of a patient’s nose or mouth mucosa.
Those unique SARS-Cov-2 RNA strands are what COVID-19 tests screen for; if they’re present, the patient is infected with the novel coronavirus. But viral RNA extraction kits weren’t available—suppliers were backordered for at least eight weeks, the team quickly found. So, they got scrappy. “We knew there were other reagents we could use,” Murphy says.
They knew that all across the BU Medical Campus, tons of labs had stockpiles of broad-use RNA extraction kits. RNA, which stands for ribonucleic acid, is essential to all organic life—it provides instructions for cellular machinery to manufacture the proteins that make up the structures of all cells, tissues, and organs. (Viruses don’t have cells of their own; instead they are made up of pieces of RNA encased in proteins. So, they rely on infecting animal and human cells to take advantage of their host’s cellular machinery, tricking them into reading the viral RNA instructions to build more copies of the virus—much to the host’s peril.) Studying RNA, therefore, is essential to understanding how humans stay healthy or develop disease. To do that, scientists need to isolate RNA from cells using a variety of standard RNA extraction kits.
“I don’t want to say the government failed, but there was a letdown in the kits being shipped to BMC…”
Murphy reached out, across the Charles River, to friend and fellow scientist Pardis Sabeti and her research team at the Broad Institute for their help working through the problem. “We were asking, ‘How would you do this with various reagents?’ We were working out the supply chain issues, identifying which reagents we were able to come by,” Murphy says.
Not only did they want to pick something that would work now, they also wanted a reagent they wouldn’t run out of in the coming weeks or months.
“We decided to go with using a very basic RNA extraction kit, we knew everyone would have it in their labs, so we plugged that into our EUA application,” Murphy says. The team put out the call to their colleagues across the BU Medical Campus, and kit donations came flooding in.
The problem with using a non-viral-specific kit, however, is that it liberates all the RNA within a cell, not just RNA from a virus. That muddies the waters, making it necessary to sift through lots of normally-occurring levels of human RNA, which keep our cells functioning properly, to find any amount of SARS-CoV-2 RNA. Just like any diagnostic test, a coronavirus test requires there to be a certain threshold of SARS-Cov-2 RNA to trigger a result. “You’ve got to be able to get enough viral RNA from a sample to amplify and detect it,” Murphy says.
Working around the clock
In the CReM, the team barely took breaks for sleep. Graduate students, faculty, postdoctoral researchers, staff technicians—it was all hands on deck. Richard Giadone, a BU graduate researcher days away from defending his PhD dissertation over Zoom, was there around the clock. “He was a critical part of the development team that created an FDA-approved COVID-19 test in one week,” Murphy says.
A CReM conference room became mission control, where researchers worked out new strategies to try optimizing the basic RNA extraction kit into a workable process for isolating SARS-Cov-2 RNA. On the table, coffee and snacks were strewn about, the team working so frantically they went without square meals for days. On the walls, whiteboards quickly filled with promising calculations and notes for troubleshooting each attempt. In the lab, researchers kept trying out each newly-conceived combination of techniques in hopes of developing a suitable protocol with the limited resources available.
“Our day job is to make stem cells, not diagnostics,” Murphy says. “It’s like we turned the CReM into a startup company to solve this problem. All the while, we’re working from separate rooms to maintain social distancing, never more than three people at a time in the same area.”
Within days, the team discovered that 150 microliters of RNA extraction solution, combined with other ingredients and several hands-on steps, generated enough viral RNA for detecting SARS-CoV-2.
“We made a brute-force RNA extraction process, we’re running the samples through spin columns, washing and pipetting samples into [PCR] plates,” Murphy says. PCR stands for polymerase chain reaction, a process that happens inside a lab machine—called a thermocycler—to make millions or billions of copies of genetic material. In this case, it multiplies the amount of viral RNA in a sample to a high-enough quantity that a test can detect SARS-CoV-2 from just a handful of a patient’s cells, originally captured by cotton swab.
A CReM bioinformatician, Taylor Matte, wrote a software script that allows the team to read off test data coming directly out of the thermocycler, allowing them to tentatively see a result before the sample gets sent up four floors to BMC pathology, where results are formally confirmed by clinicians.
“It takes a village,” Murphy says. “We started off with people from my own CReM group, but we knew immediately that we needed more people, so we started onboarding more help.” Behind the scenes, from the isolated safety of their homes, volunteers mobilized to recruit other researchers accustomed to running PCRs for their own experiments.
Molecular biologists from all over campus have stepped forward, getting cleared by BMC’s human resources department to work with clinical samples. “You can’t just show up and do it, you have to become a BMC-vetted employee,” Murphy says. “There are procedural things that need to happen to transform a basic scientific researcher into a clinical laboratory technician.”
Before they can work with real patient samples, BMC has to check their health history and make sure their vaccinations are up to date. Dozens upon dozens of these volunteers, once vetted, will staff the CReM around the clock so the inhouse COVID-19 tests keep pouring out results. All the while, just down the street, BMC clinicians will use those rapid-turnaround results to make decisions that could save lives.
“I don’t want to say the government failed, but there was a letdown in the kits being shipped to BMC,” Murphy says. “It’s science at its finest when collaborators get together to develop inhouse protocols, using their expertise, to directly impact patient care during a public health emergency.”
Most importantly, he says, in line with the CReM’s philosophy of doing “open source” biology and making its data available to all, the inhouse coronavirus test protocols developed by the team are now freely available to the worldwide scientific community.
Murphy says anyone interested in the protocols can reach out on Twitter: @DrGJMurphy.
Source: Boston University
The post Team creates their own coronavirus test to fill gaps appeared first on Futurity.
Share this article:
This article uses material from the Futurity article, and is licenced under a CC BY-SA 4.0 International License. Images, videos and audio are available under their respective licenses.
Related Articles:
More staff COVID testing saved nursing home resident lives
March 24, 2023 • futurityNew COVID-19 test is fast, accurate, and low-cost
Feb. 1, 2022 • futurityLinks/images:
- https://www.futurity.org/covid-19-drugs-research-2313292/
- https://www.futurity.org/do-i-have-covid-19-online-tool-2315072-2/
- https://www.futurity.org/fda-approval-speed-1400212-2/
- http://www.bu.edu/dbin/stemcells/open_source_biology.php
- https://twitter.com/DrGJMurphy
- http://www.bu.edu/articles/2020/crem-coronavirus-test/
- https://www.futurity.org/coronavirus-test-2320152/
- https://www.futurity.org